CHAMPS RESOURCES
CHAMPS Resources
An early neonate who died of hyaline membrane disease, complicated by bilateral pneumothorax, premature birth and maternal hypertension
An HIV-positive mother gave birth to a 30-week-old baby girl upon arriving at the hospital with gestational hypertension. Due to her high blood pressure and detected fetal distress, the baby was born prematurely via C-section.
At delivery the baby presented a weak cry, irregular breathing, bluish discoloration of the hands and feet. She was treated with supplemental oxygen and continuous positive airway pressure (CPAP) ventilation to assist breathing efforts. The baby responded well to the intervention but required continued monitoring for hyaline membrane disease, also commonly referred to as respiratory distress syndrome (RDS).
On the first day of monitoring, the baby’s oxygen dropped, and she stopped breathing which required ventilation suctioning. She recovered and eventually was placed back on the CPAP machine to help with breathing.
By the third day, the baby had additional sleep apneas that required reintubation and intermittent positive pressure ventilation. A small swelling was observed on the back of the baby’s neck, suggesting a pneumothorax (air being around or outside of the lung) or collapsed lung, indicating the airway was decompressed. Although she initially recovered, her heart rate and blood pressure dropped, and a second collapsed lung was suspected.
Despite continuous interventions, the baby went into cardiac arrest, was resuscitated and placed on an oscillator, but ultimately did not respond and died at the hospital at three days old.
Uncovering the Cause
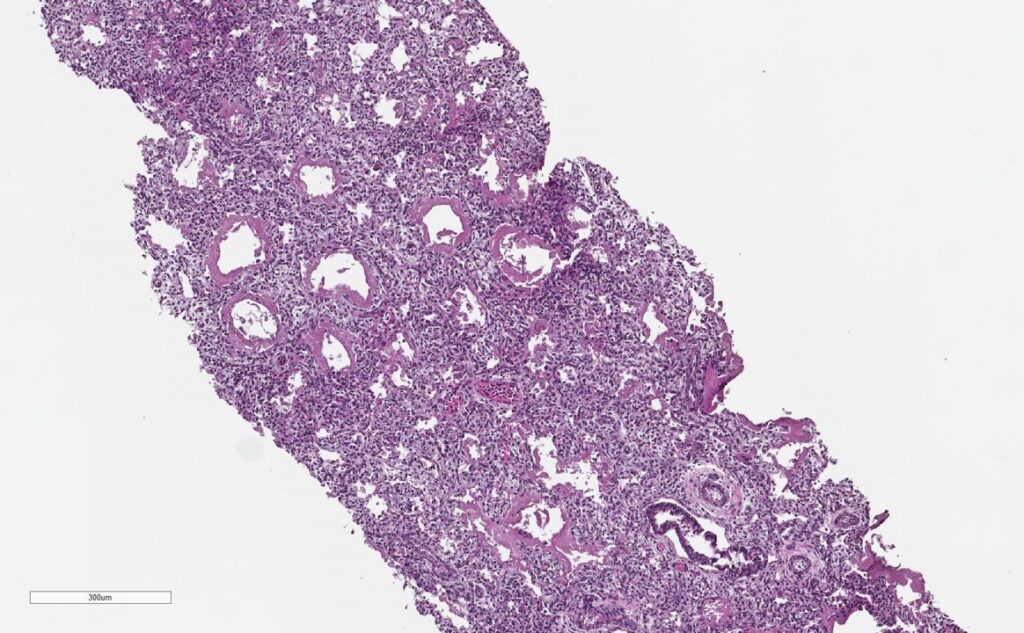
All CHAMPS laboratory results were negative for possible infectious causes of death in this case. Pathology from the baby’s right and left lungs showed severe hyaline membranes and mild interstitial inflammation, confirming the presence of RDS.


Note the thick pink membranes lining the alveolar spaces (arrows)
The CHAMPS team determined the baby died from complications of bilateral pneumothorax due to RDS. It is likely that maternal hypertension caused the premature labor.
Public Health Implications
According to the World Health Organization, 15 million babies are born prematurely (i.e., live birth occurring before 37 weeks of gestation) every year across the globe. More than 60% of preterm births occur in low- and middle-income countries in Africa and South Asia.
Infant RDS is one of the most common complications in premature babies, caused by lack of surfactant fluid that serves to reduce tension of pulmonary fluids and prevent collapsed lungs. Preventing RDS requires early and consistent ANC visits (WHO recommends at least 8 during pregnancy) to help establish a routine of care and give physicians the best chance of identifying possible preterm labor risks; if caught early, physicians can prevent or reduce the severity of RDS by administering antenatal corticosteroids (ACS) to promote healthy lung development.
For maternal hypertension, the Centers for Disease Control and Prevention recommends women talk with their doctors before getting pregnant so they can be prescribed an appropriate treatment and get blood pressure levels under control. Antenatal care (ANC) visits are important in every pregnancy, but early and regular visits for mothers with high blood pressure are vital to avoid preterm labor.
Implementing Data to Action
Under-5 mortality data collected across CHAMPS sites remains consistent, but recent findings now inform expanded data collection efforts that include pregnancy surveillance. This will include implementing a pregnancy notification system for each catchment area’s community and health facilities, ensuring there are up-to-date records of pregnant women in the area. These records will be important in the facilitation of at-home ANC visits or facility referrals when needed throughout pregnancy and 12 months postpartum.
New developments in RDS treatment include a non-invasive lung surfactant that could prevent deaths like this case; these surfactants provide adequate respiratory therapy while minimizing the risk of lung injury associated with more traditional intubation and ventilation.
Again, early ANC is crucial to identify possible preterm labor risks and encourage pregnant women to utilize in-facility delivery services. Health facilities with advanced technology will be able to provide superior newborn care including continuous positive airway pressure (CPAP) treatment which is necessary for delivering innovative non-invasive lung surfactant treatments.
While CPAP alone can reduce case fatality of RDS to 30%, additional treatment from non-invasive surfactant may be able to reduce RDS case fatality to 12%. As this option is more frequently implemented, future ANC practice should include referring women with risky pregnancies to CPAP-equipped facilities, ideally with the capability of using non-invasive surfactant treatments as part of newborn care.
Interested in more CHAMPS updates?
Email data@champshealth.org for information about CHAMPS pathology slide images.